Individuals often fail to invest in preventive healthcare, even when such investments cost little and individuals are aware of their benefits. An estimated two thirds of deaths of children under five could be averted with cheap preventive technologies (like malaria bednets, vaccinations, and oral rehydration salts). A prominent example is chlorination of drinking water, which is highly effective in reducing prevalence of diarrhoea, particularly among young children. Diarrhea is the second leading cause of death worldwide among children aged 1–5, contributing to nearly half a million deaths in 2015. It also stunts healthy growth in children by preventing nutrients from being absorbed. In many settings, chlorine for water is readily and cheaply available, but infrequently used by individuals without access to clean water. In our study areas in Kenya, only three percent of households used chlorine before any intervention, although a month's supply costs only KES 25 (USD 0.25). Interventions which provide chlorine for free, often in combination with information or marketing campaigns, increase usage somewhat, but take-up remains far below complete.
Researchers study the role of behavioural barriers to drinking water chlorination: People may not value future benefits enough (patience), they might be unaware of the benefits (information), they may not believe in their own ability to achieve desirable outcomes (self-efficacy), or they might be unable to plan and remember to chlorinate (planning skills). Using a randomised experiment in rural Kenya, researchers test the effect of two psychological interventions (group workshops) on both health and economic outcomes. One intervention encourages participants to visualise alternative realisations of the future; one builds participants' ability to make concrete plans.
This study was run in 205 villages in Western Kenya (Bungoma and Kakamega) with with 3,750 women. Researchers recruited women of childbearing age (18–35), because small children are the most vulnerable to water-borne illnesses. The interventions were implemented as group workshops with five participants, with two sessions lasting two hours each. Workshops featured a mix of interactive lectures, case stories, and exercises.
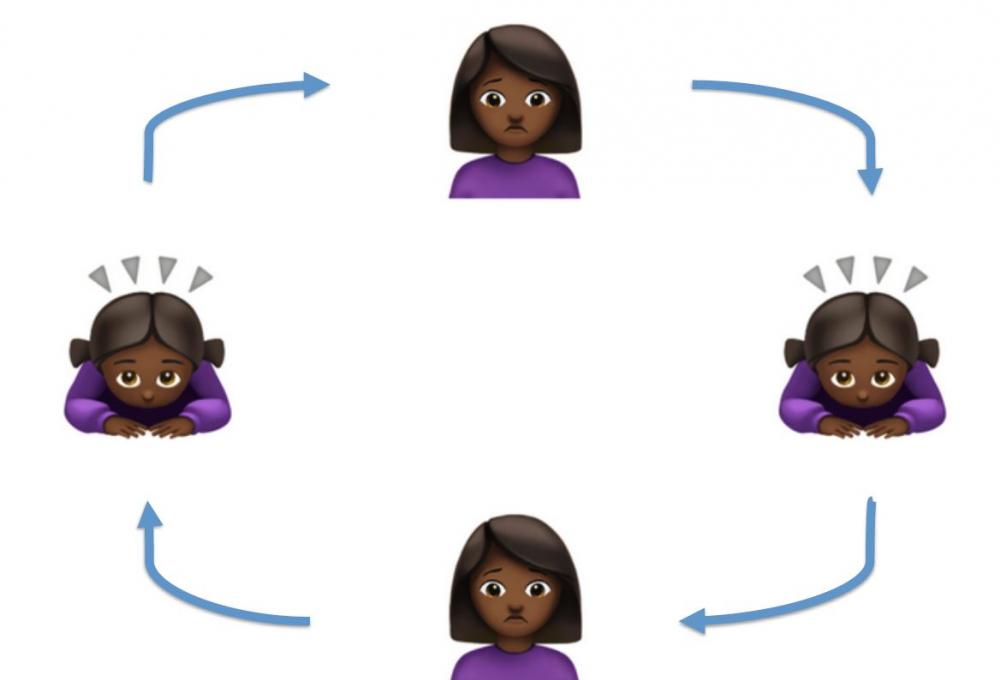
The participants were allocated to four treatment arms: In the first group, participants visualised alternative realisations of the future, depending on their behaviour in the present (“Visualisation” or “V”). The intervention aimed to make future outcomes more vivid and tangible in participants' minds, thus increasing their perceived value relative to the more immediate costs required to attain them. The second group aimed to build participants' ability to make concrete, specific plans, anticipate potential obstacles, and establish routines (“Planning” or “P”). Both interventions required participants to think about how their current behaviour affects their future outcomes. To isolate the effects of the psychologically active elements of these treatments, a third, active control group received all elements of the intervention except the psychologically active components (“Active Control” or “AC”). In addition, all three groups received a short information module about the benefits of chlorination, to hold beliefs about chlorination constant across groups. Researchers compare these treatments to a fourth, pure control group (“PC”), who were simply surveyed at endline. The comparison between the two “psychological” treatment groups (Visualisation and Planning) relative to our Active Control identifies the effect of psychological interventions, over and above interventions targeting a lack of information. The comparison between the three “active” treatment groups and our pure control identifies the policy-relevant total effect of providing interventions like ours.
Twelve weeks after the interventions, researchers conduct unannounced household visits, in order to objectively measure whether participants chlorinate their drinking water. An additional endline survey measures health outcomes (like children's diarrhea) and economic outcomes (like savings). To understand the mechanisms for the treatment effects, researchers use state-of-the-art incentivised elicitations of psychological targets, including time-preferences, self-efficacy, and planning skills.
The visualisation intervention increased chlorination of water, decreased child diarrhea episodes, and was cost-effective. Effects extended to non-health outcomes, including savings and labour supply, and were visible almost three years after the initial intervention. By contrast, the planning intervention had minimal impacts.
Visualisation increased chlorination of household drinking water and was effective at decreasing diarrhea episodes: Twelve weeks after the first session, the share of households in the Visualisation group whose drinking water contained chlorine increased by five percentage points from a base of 23 percent (a 22 percent increase). After almost three years, when asked an unprompted question about how they treat their water, participants in the Visualisation group were five percentage points more likely to state that they chlorinate it (a six percent increase from a base of 85 percent). The number of diarrhea episodes per child under the age of five in the Visualisation group decreased by 0.16 episodes, from a base of 0.34 episodes (a 47 percent decrease) after ten weeks. This effect did not persist over time, although this may have been due to seasonal effects, as the long-run data collection occurred during the dry season, when diarrhea is more likely to be caused by airborne viruses. By comparison, the Planning intervention had positive but insignificant effects on objective chlorination measures and no impact on diarrhea outcomes for children under five years of age after 10-12 weeks.
The Visualisation intervention was also cost-effective: Delivery of the intervention costs approximately $4 per household. The estimated cost per Disability-Adjusted Life Year (DALY) saved ranges between $62 and $248, depending on assumptions about the duration of the effect on diarrhea, and on whether benefits to children under five or 15 years old are considered. The estimates are well within the WHO’s highly cost-effective category (up to $1508).
Information raised knowledge on chlorination: The information module about the benefits of chlorination slightly improved participants’ beliefs about the effectiveness of chlorination in preventing pediatric diarrhea. Participants of the active intervention groups (who received the information module) showed 0.08 SD higher beliefs than participants in the pure comparison group (who did not receive information). However, changes in information did not explain the observed increases in chlorination: participants in the active comparison group did not show higher rates of chlorination than participants in the pure comparison group. Such effects are only observed in the group who additionally received the Visualisation treatment.
Visualisation and planning both led to greater beliefs in ability to achieve desired outcomes: After ten weeks, both the Visualisation and the Planning groups showed increases in the belief that they are able to achieve desirable outcomes and overcome obstacles - a concept that psychologists call "self-efficacy." It was measured by asking participants' agreement to statements like “I always manage to solve difficult problems if I try hard enough.” This result showed that both Visualisation and Planning interventions strengthened the connections that participants make between their behaviour in the present and desired outcomes in the future. While both groups were affected, the observed effects were stronger and more long-lasting in the Visualisation group. After 30 to 36 months, participants in the Visualisation group maintained higher levels of self-efficacy than those in the Planning group (0.14 SD difference), consistent with the differential long-term effects on chlorination. Furthermore, participants in the Visualisation group were better at vividly imagining themselves and their family in the future. There were no detectable differences between the groups in time preferences over effort or money, planning skills, or attitudes toward risk.
Visualisation also had impacts on non-health outcomes: The Visualisation and Planning treatments were not specific to chlorination, but considered many examples of daily behaviour, inspired by the participants'; own ideas. Visualisation led to a higher amount of money saved regularly per week. This effect persisted after almost three years, by which point the Visualisation group had accumulated 41 percent higher savings. Visualisation participants also joined more rotating savings and credit associations, and saved more for productive investments (education, business, agriculture). Beyond savings outcomes, Visualisation participants worked 2.3 hours more in the last seven days than comparison participants, on a base of 13 hours (an 18 percent increase), 30-36 months after the intervention. A likely explanation is that some participants used the Visualisation sessions to develop longer-term career visions, including applying for salaried jobs. This increased their labor supply in the long-run.