We look at whether the conditional cash transfer Program Keluarga Harapan (PKH) in Indonesia reduced the suicide rates. PKH was designed to improve poor households’ health and education through a cash transfer, conditional on their children’s participation in health and education services.
Publication Available: Cornelius Christian, Lukas Hensel, Christopher Roth; Income Shocks and Suicides: Causal Evidence From Indonesia. The Review of Economics and Statistics 2019; 101 (5): 905–920. doi: https://doi.org/10.1162/rest_a_00777 |
Suicide is a pressing public health concern, causing 800,000 deaths per year globally (WHO, 2014). Furthermore, suicidal behaviour is one of the leading causes of death for people with severe mental illness (Hawton et al., 2013). At the same time, poverty alleviation programmes in the shape of conditional and unconditional cash transfer programs have been implemented in many developing countries. While the effects of these programs on consumption, health and education have been thoroughly evaluated, there is little known about their effects on suicides, a particularly dire consequence of poverty and mental health problems. In particular, there is very little causal evidence linking positive income shocks to suicidal behaviour in developing countries (Alves et al. 2019 constitute a rare exception).
There is good reason to hypothesize that poverty alleviation programmes should reduce suicides. Indeed, previous research has found a causal link between poverty and suicidal behaviour (Carleton, 2017), and this effect could be driven by poverty’s effect on mental health and in particular depression (Haushofer and Fehr, 2014; Schilbach et al., 2016). However, poverty could also have a direct effect on suicides by increasing stress levels and changing social circumstances. Since cash transfers reduce stress and mental health problems (Baird et al., 2011; Haushofer and Shapiro, 2016), they might also reduce suicide rates.
In the Program Keluarga Harapan (PKH), households needed to fulfill one of the following program criteria in order to be deemed eligible for a cash transfer: (i) households with pregnant and/or lactating women; (ii) households with children aged 0-15 years; (iii) households with children aged 16-18 years who have not yet completed 9 years of basic education. Only the subset of eligible households with the lowest predicted consumption were included in the program. In the end, approximately 10% of all households in targeted sub-districts were included in the programme.
Treated households received between 39 and 220 US dollars per year. The average received amount constituted about 10% of pre-PKH yearly household expenditure (80.82 US dollars at 2005 prices) between 2007 and 2014. A pilot version of the PKH was introduced in 2007 for 600,000 households, and the programme was then expanded to cover 5.2 million households in 2014, with a target of 10 million recipients in 2018.
Researchers exploit this roll-out using a difference-in-differences specification to estimate the effect of the programme on suicides. At its launch in 2007 it covered 13% of Indonesian sub-districts in seven provinces. The programme was widely expanded, reaching 57% of sub-districts across all 33 provinces in 2013. This provides researchers with sufficient variation in exposure to PKH to study the impact on suicides. Specifically, researchers use two stages of the roll-out to identify variation: the first stage of sub-districts who received the treatment from 2007 to 2011, and the second stage of sub-districts who received the treatment in 2012 and 2013. To measure the suicide rate, researchers leverage village-level census data on every Indonesian village from 2000 to 2014, aggregated at the subdistrict level. Specifically, researchers have three pre-treatment periods (2000, 2003, 2005) and two post-treatment periods (2011 and 2014) available. This allows them to study pre-trends, to provide evidence that sub-districts’ trends in suicides did not diverge prior to receiving the PKH programme. The wide scope of the data is necessary to have the power to study rare events such as suicides. The results from a randomised controlled trial of the same program are less powered, but very much in line with the difference-in-differences results.
To study whether the program also mitigated the effects of droughts, researchers explore plausibly exogenous rainfall variation. As much of rural Indonesia relies on rain-fed agriculture, rainfall provides a good proxy for income shocks of poor parts of the population. Researchers leverage data on depression from the Indonesian Family Life Survey (IFLS) to confirm that, as we would expect, droughts indeed affect consumption and depression scores.
The main result obtained shows that the PKH program reduced the suicide rate by 0.36 suicides per 100,000 people (18 percent). Given that the program only targeted the poorest ten percent of the population, this suggests an important role of positive spillover effects on non-beneficiaries (in line with the medical literature on suicides). In absolute numbers, researchers estimate that the PKH program prevented about 1,065 suicides, which amounts to one suicide for every 672,000 USD spent.
Researchers also study the shape of the relationship between income and suicides and draw the following three conclusions. First, the PKH program is most effective at reducing suicides when income levels are low. As the income level increases, its effectiveness reduces. Second, they find no evidence of adaptation effects over time. This is important as it suggests that the effectiveness of conditional cash transfer programs does not diminish over time. Third, they estimate that the PKH programme was much more effective in reducing suicides per dollar spent than equivalent rainfall shocks. They speculate that this could be driven by the predictability of the payments, which might reduce stress and increase their current consumption value.
Researchers also find that droughts affect suicides. A one standard deviation decrease in rainfall increases the suicide rate by 0.8 suicides per 100,000 population. This relationship disappears in sub-districts that receive the PKH program, suggesting an important role for policy in mitigating the consequences of negative income shocks.
Finally, researchers provide suggestive evidence that the relationship between economic circumstances and suicides could be mediated by mental health. Using panel data from the Indonesian Family Life Survey, they show that droughts causally affect farmers’ mental health. A one standard deviation increase in sub-district level rainfall increases consumption by approximately seven percent, and reduces depression by 0.12 of a standard deviation. Moreover, the relationship between rainfall and depression is absent for non-farmers, indicating that the effects of rainfall operate through an economic channel.
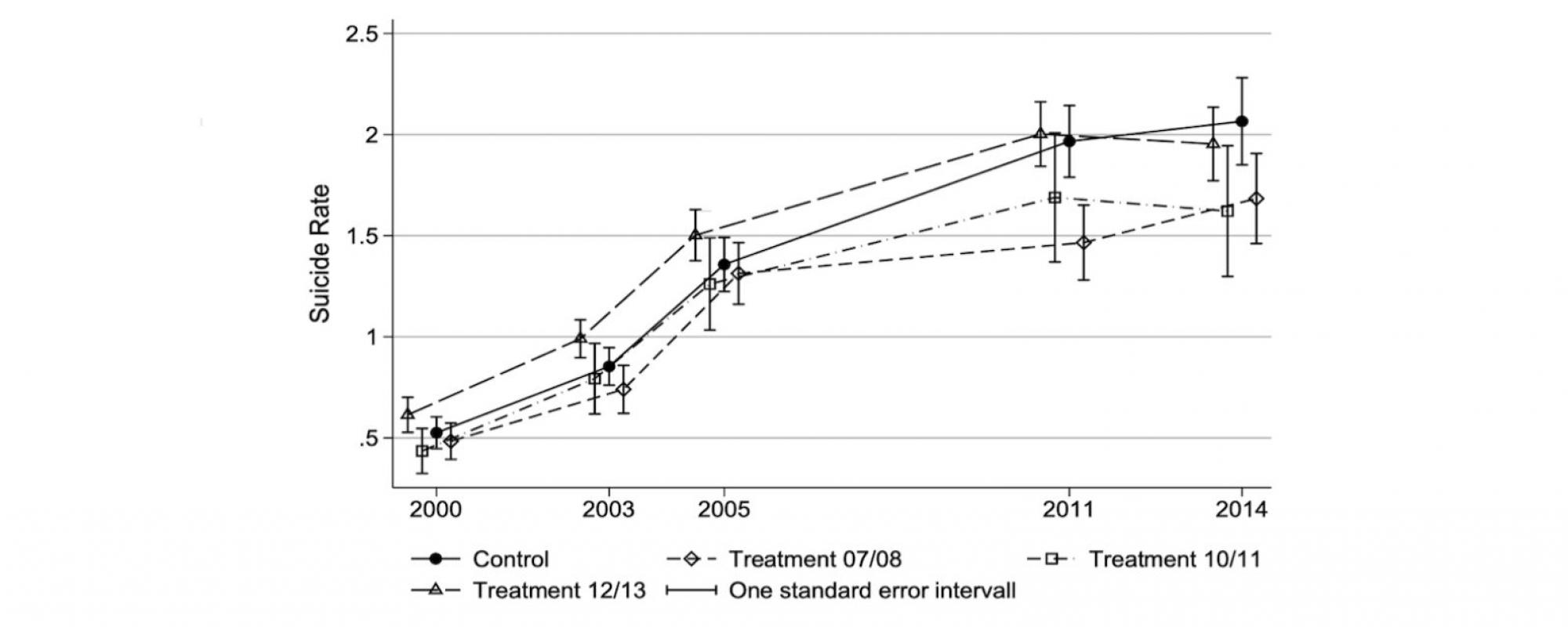
Figure 1 displays mean suicide rates over time for different treatment groups. It clearly shows that suicide rates developed in parallel prior to the receiving the PKH program. Sub-districts receiving the PKH program then showed a significantly smaller increase in suicides than the control group.
Alves, F. J. O., Machado, D. B., & Barreto, M. L., “Effect of the Brazilian cash transfer programme on suicide rates: a longitudinal analysis of the Brazilian municipalities,” Social Psychiatry and Psychiatric Epidemiology, 2019, 54 (5), 599-606.
Baird, Sarah, Craig McIntosh, and Berk Ozler, “Cash or Condition? Evidence from a Cash Transfer Experiment,” The Quarterly Journal of Economics, 2011, 126 (4), 1709– 1753.
Carleton, T., “Crop-Damaging Temperatures Increase Suicide Rates in India,” Proceedings of the National Academy of Sciences, 2017, 114 (33), 8746–8751.
Haushofer, Johannes and Ernst Fehr, “On the Psychology of Poverty,” Science, 2014, 344 (6186), 862–867.
Hawton, Keith, Carolina Casanas i Comabella, Camilla Haw, and Kate Saunders, “Risk Factors for Suicide in Individuals with Depression: a Systematic Review,” Journal of Affective Disorders, 2013, 147 (1), 17–28.
Schilbach, Frank, Heather Schofield, and Sendhil Mullainathan, “The Psychological Lives of the Poor,” American Economic Review: Papers and Proceedings, 2016, 106 (5), 435–40.
WHO, “Preventing Suicide: A Global Imperative,” Geneva: World Health Organization, 2014.
